Scientists discover a ploy used by multiple pathogens to thwart cellular defenses, offering a new strategy for antiviral development.
LA JOLLA, CA—An attack mechanism that influenza and other viruses use to defeat a host defense system in cells could be targeted with a single drug, presenting a rare opportunity to protect people from multiple viral infections at once, a new study from the lab of Sumit Chanda, PhD, shows.
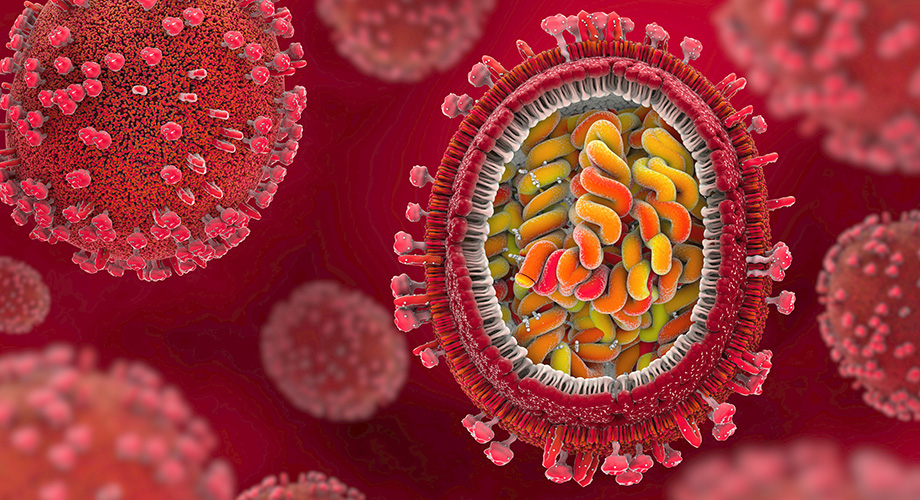
Chanda and colleagues, whose findings appear today in Nature Microbiology, used painstaking methods to find this point of potential vulnerability. They started by cataloging genes and other cellular factors that defend human cells from influenza A viruses, a group known to cause pandemics. After generating more than 100 clues with their initial screen, the researchers investigated one in detail, revealing how the virus disables a key cell defense system called autophagy. Autophagy is a process cells use to expel and reprocess waste.
“This may turn out to be an important mechanism not just for flu but also for SARS-CoV-2 and a lot of other viruses—and targeting this mechanism could be a new and better approach to antiviral treatment,” says study senior author Sumit Chanda, PhD, a professor joining the Department of Immunology and Microbiology at Scripps Research and an investigator in Scripps Research’s nonprofit drug discovery and development division, Calibr.
Chanda recently moved to Scripps Research from the Sanford Burnham Prebys Medical Discovery Institute, where this study was conducted.
SARS-CoV-2 and flu viruses have killed millions of people, yet at present there are limited options for drug treatment. Part of the challenge is how rapidly viruses mutate to evade drugs and vaccines. In the quest for a vulnerability that would persist, Chanda worked with first author Laura Martin-Sancho, PhD, a postdoctoral research associate, plus collaborators at the University of California-San Francisco, University of California-San Diego, and Icahn School of Medicine at Mount Sinai. The team cast a wide net by looking for human genes, proteins, and RNAs whose deletion or depletion would improve these viruses’ ability to replicate in cells.
Among the many leads was a protein called TBC1D5. It has been known to play a key role in the cellular garbage disposal system autophagy. Cells use the system to engulf and destroy not only malformed proteins and other ordinary cellular waste matter, but also invading viruses. Martin-Sancho and the team showed in detail how an influenza A virus protein called M2 interacts with the TBC1D5 protein to disrupt the normal operation of this garbage disposal system, thus allowing flu virus particles to escape infected cells, and go on to infect other cells much more efficiently than they would otherwise.
In recent years, evidence has accumulated that cells use autophagy to help them defend against infections by a broad set of viruses. These include HIV and coronaviruses. Chanda concluded that the viruses must somehow thwart that defense system to sustain their efficient spread. Thus, flu viruses’ disruption of autophagy is an important part of the “arms race” between viruses and their animal hosts, pointing to a promising strategy for broadly acting antiviral treatments, Martin-Sancho says.
“We think that blocking this attack mechanism could be not only effective against many viruses but also relatively easy and safe, since we’d be merely helping our cells to do better what they do anyway when infected,” Martin-Sancho says.
Next steps are to further study the details of the M2-host protein interaction, and to launch a hunt for potential drugs to block it and restore efficient autophagy in virus-infected cells. They also plan to investigate other leads among the hundreds they catalogued.
“We think that this dataset we generated is going to be a valuable resource for the virology community, for understanding influenza virus and for generating new antiviral strategies,” Chanda says.
In addition to Chanda and Martin-Sancho, the study, “Restriction factor compendium for influenza A virus reveals a mechanism for evasion of autophagy,” was co-authored by Ariel Rodriguez-Frandsen, Lars Pache, Laura Riva, Courtney Nguyen, Nish Beltran-Raygoza, Stephen Soonthornvacharin, and Paul de Jesus, all of the Sanford Burnham Prebys Medical Discovery Institute at the time of the research. Other co-authors are Shashank Tripathi, Maite Sanchez-Aparicio, Guojun Wang, Randy Albrecht and Adolfo García-Sastre of Icahn School of Medicine at Mount Sinai; Michael McGregor, Kelsey Haas, Danielle Swaney, Thong Nguyen, David Jimenez-Morales, Judd Hultquist and Nevan Krogan, of the University of California, San Francisco; Christopher Churas, Dexter Pratt, Sara Rosenthal, Max Chang, Chris Benner and Trey Ideker of the University of California, San Diego; João Mamede of Rush University Medical Center, and Hong Moulton and David Stein of Carlson College of Veterinary Medicine.
The research was supported by the National Institutes of Health (U19AI106754, U19AI135972, U19AI117873, HHSN272201400008C, K22 AI136691), the James B. Pendleton Charitable Trust, the National Science Foundation (1650113), and the Gilead Sciences Research Scholars Program in HIV.