Even though the viruses that cause SARS and COVID-19 are closely related and infect cells the same way, they aren’t cross-protective in cell culture experiments.
LA JOLLA, CA — COVID-19 isn’t the first serious disease to be caused by a coronavirus, and it likely won’t be the last. That’s why scientists at Scripps Research and around the world are investigating whether a single vaccine can be designed to protect against many coronaviruses, including those that have not yet emerged.
In a study published in Cell Reports, researchers at the University of Hong Kong and Scripps Research explored whether antibodies produced in response to one coronavirus might be protective against a different type of coronavirus—knowledge that could offer important clues to creating a broadly effective vaccine. Specifically, they tested the cross-protective properties of antibodies from SARS-CoV, which causes SARS (severe acute respiratory syndrome) and SARS-CoV-2, which causes COVID-19.
In experiments involving cell cultures, the team found that while the antibodies from one coronavirus could bind to the other coronavirus, the cross-reaction wasn’t enough to disable—or neutralize—the other virus.
“It was a bit surprising to see the prevalence of cross-reactive, yet non-neutralizing antibody responses,” says Nicholas Wu, PhD, co-first author at Scripps Research.
However, it remains unclear whether the findings from the cell culture reflect what would happen in the human body. One possibility is that cross-reactive, non-neutralizing antibodies do offer protection against other coronaviruses in the body, even though they don’t protect cultured cells. This phenomenon has been observed for other types of viruses.
On the other hand, non-neutralizing antibodies could have the opposite effect, actually enhancing the ability of other coronaviruses to infect cells and replicate through a process known as “antibody-dependent enhancement.” This has been previously reported for the SARS-causing coronavirus.
“Whether antibody-dependent enhancement plays a role in SARS-CoV-2 infection needs to be carefully examined in the future,” says co-senior study author Ian Wilson, DPhil, Hansen Professor of Structural Biology at Scripps Research and Chair of the Department of Integrative Structural and Computational Biology. “Addressing this question will be critical for developing a safe and effective universal coronavirus vaccine.”
Wilson and his team concluded that more research will be needed to identify parts of the coronavirus that are critical for inducing a cross-protective immune response.
SARS and COVID-19: How do human antibodies respond?
From late 2002 to 2003, more than 8,000 people worldwide became sick with SARS, resulting in more than 700 deaths. The virus responsible for this outbreak, SARS-CoV, shares approximately 80 percent of its genomic identity with that of SARS-CoV-2, which causes COVID-19.
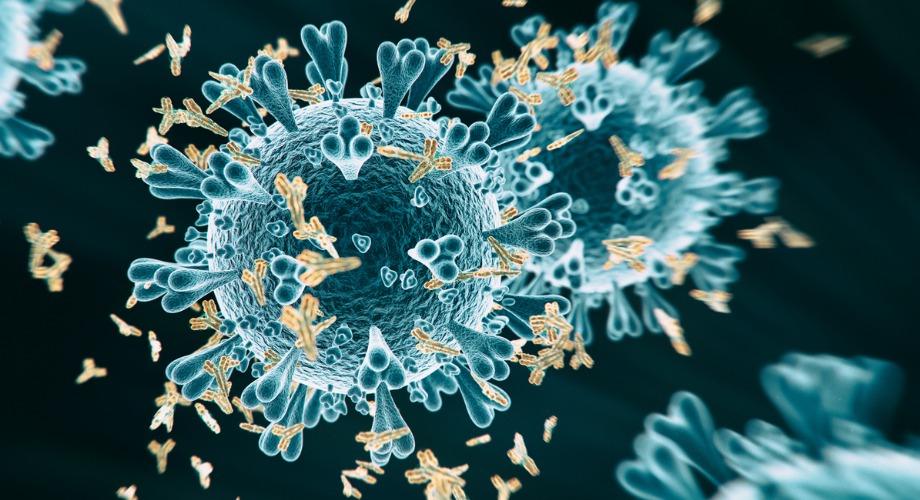
The two coronaviruses also enter and infect cells the same way using a part of the virus known as the “receptor-binding domain,” or RBD, of the spike protein. Located on the surface of the virus, the RBD binds to a human cell receptor called ACE2, enabling infection.
Past studies have shown that protective antibodies against SARS-CoV bind to the RBD to disable the virus. But relatively little was known about the antibody response to SARS-CoV-2 infection. It is also unclear how infection with SARS-CoV influences the antibody response against SARS-CoV-2, and vice versa.
Gaining insight into these questions could guide the development of an effective vaccine for COVID-19 and shed light on whether such a vaccine might cross-protect against similar coronaviruses, the scientists say.
“There are related viruses still circulating in bats, and it is unclear whether any of these may also threaten human health in future,” says co-senior study author Malik Peiris of the University of Hong Kong. “As such, whether infection by one of these viruses cross-protects against another is an important question.”
Addressing a gap in knowledge
In pursuit of answers, the researchers analyzed blood samples collected from COVID-19 patients in Hong Kong. Five samples collected from patients 11 days after symptom onset or later had antibodies capable of binding to the RBD and other parts of the spike protein on both SARS-CoV-2 and SARS-CoV.
The researchers also analyzed blood samples collected from seven former SARS patients. These samples had antibodies capable of binding to the RBD and other parts of spike protein on the COVID-19-causing virus.
Taken together, these findings show that infection with one coronavirus induces the production of antibodies that can bind to both RBD and non-RBD regions of the spike protein on the other coronavirus.
Using cell-culture experiments, the researchers next tested whether infection with SARS-CoV-2 induces SARS-CoV-2-specific neutralizing antibodies, which protect host cells by preventing the virus from interacting with them. All 11 blood samples collected 12 days or later after the onset of symptoms had neutralizing antibodies against SARS-CoV-2. But only one blood sample had cross-neutralizing antibodies against SARS-CoV, and this response was very weak. Similarly, five blood samples from patients infected with SARS-CoV had neutralizing antibodies against this virus, but none could cross-neutralize SARS-CoV-2. Additional experiments in mice supported the findings from patients.
For now, the clinical implications remain unclear. As Wilson noted, future studies will be needed to investigate whether the non-protective antibody responses seen in cell cultures reflect what actually happens in the human body.
“Since coronavirus outbreaks are likely to continue to pose global health risks in the future, the possibility of developing a cross-protective vaccine against multiple coronaviruses has been considered,” says co-senior study author Chris Mok, PhD, of the University of Hong Kong. “Our findings, albeit limited at present, would suggest that broadly cross-neutralizing antibodies to coronaviruses might not be commonly produced by the human immune repertoire.”
This work was supported by the Pasteur International Network Association, the U.S. National Institutes of Health, the Bill and Melinda Gates Foundation, Guangzhou Medical University, the National Natural Science Foundation of China and the Hong Kong Special Administrative Region, China.
Authors of “Cross-reactive antibody response between SARS-CoV-2 and SARS-CoV infections” include Huibin Lv, Nicholas C. Wu, Owen Tak-Yin Tsang, Meng Yuan, Ranawaka A.P. M. Perera, Wai Shing Leung, Ray T.Y. So, Jacky Man Chun Chan, Garrick K. Yip, Thomas Shiu Hong Chik, Yiquan Wang, Chris Yau Chung Choi, Yihan Lin, Wilson W. Ng, Jincun Zhao, Leo L.M. Poon, J. S. Malik Peiris, Ian A. Wilson and Chris K.P. Mok.